Introduction
Recurrent patellar dislocation is characterized by repeated episodes of knee cap displacement, often resulting in cartilage lesions and chronic symptoms. Traditional management approaches often yield limited success, necessitating innovative treatments such as mesenchymal stem cell (MSC) therapy.
Case Presentation
Patient History and Examination
A 21-year-old male presented with left knee discomfort following recurrent patellar dislocations over ten years. Physical examination revealed anterior knee pain exacerbated by activities like stair climbing and exercise. Diagnostic imaging confirmed significant cartilage defects, classified as Grade 3 according to ICRS standards.

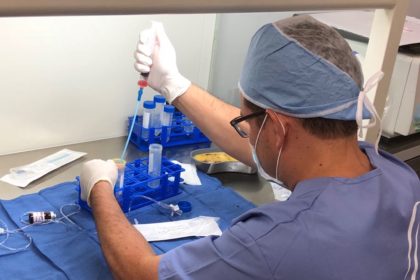
Surgical Intervention
The patient underwent arthroscopic microfracture and autologous bone marrow-derived MSCs implantation following Fulkerson osteotomy. Surgical procedures included lateral retinaculum release and tibial tubercle realignment to stabilize the patella.


Treatment Outcome
Postoperative Recovery
Post-surgery, the patient achieved full range of motion and began weight-bearing exercises. Eighteen months later, MSC implantation facilitated significant cartilage growth, improving International Knee Documentation Committee (IKDC) and Visual Analog Scale (VAS) scores.
Long-term Assessment
Two years post-MSC treatment, the patient reported no knee complaints and maintained full range of motion. MRI confirmed substantial cartilage regeneration in previously damaged areas.

Discussion
Challenges in Management
Recurrent patellar dislocations pose challenges due to high recurrence rates and associated cartilage damage. Treatment strategies like Fulkerson osteotomy combined with MSC therapy offer promising outcomes for severe cases.
Role of MSC Therapy
MSCs demonstrate potential in cartilage regeneration due to their chondrogenic differentiation capabilities and anti-inflammatory properties. This case highlights the efficacy of MSC therapy in managing extensive cartilage defects.
Conclusion
Combining Fulkerson osteotomy with MSC implantation represents a viable treatment option for chronic patellar instability and associated cartilage lesions. The integration of microfracture and MSC therapy supports significant cartilage regeneration and functional recovery.



