Platelet-Rich Plasma For Bone Healing: Myth or Fact?
WEDNESDAY, 11 APRIL 2018 / PUBLISHED IN BLOG
Platelet-Rich Plasma (PRP) has a proven record for healing soft tissues and other living tissues. But can it actually heal bones? This could mean PRP, when applied to an affected area such as an elbow joint, knee, or backbone area, heals everything within its reach, including bones. Is that really why PRP works? Let’s examine.
Platelet-Rich Plasma for Bone Healing
Bones are not just lifeless matter attached to living tissues. They are as much living as the tissues themselves and are constantly changing. Old bone cells are broken down and replaced with new ones in a three-part process called bone remodeling. This involves resorption (digestion of old bone cells), reversal (birthing of new cells), and formation (new cells turn into fully formed bones).
This process, like other biological processes in the body, requires hormones and growth factors. Some of these include parathyroid hormone (PTH), calcitriol, insulin-like growth factors (IGFs), prostaglandins, tumor growth factor-beta (TGF-beta), bone morphogenetic proteins (BMP), and cytokines. For this discussion, we need to remember only one thing: a large number of cytokines and growth factors are involved in the bone remodeling process. This means we can accelerate the bone remodeling process by supplying these cytokines and growth factors as suggested by various studies.
Why Platelet-Rich Plasma?
Autologous Platelet-Rich Plasma (PRP), being completely “whole and natural,” can more closely simulate a highly efficient in-vivo situation than anything else made up of artificial recombinant proteins. In PRP, we take advantage of the biological benefits of growth factors whose functions we know as well as those we do not know yet. From the 15+ factors we know are in PRP, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-beta), platelet factor 4 (PF4), interleukin 1 (IL-1), platelet-derived angiogenesis factor (PDAF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), platelet-derived endothelial growth factor (PDEGF), epithelial cell growth factor (ECGF), insulin-like growth factor (IGF), osteocalcin (Oc), osteonectin (On), fibrinogen (Fg), vitronectin (Vn), fibronectin (Fn), and thrombospontin-1 (TSP-1), we’re supplying a “holistic” set of nutrients for healing that cannot be mimicked by those obtained artificially.
PRP: Organic Fertilizers for the Body
The difference with PRP is akin to adding chemical fertilizers versus organic fertilizers to plants. Chemical fertilizers are rich in essential nutrients that we know are needed for crops. On the other hand, organic fertilizers supply nutrients not only to the plants but also to the soil, improving the soil structure and tilth, water-holding capacity, reducing erosion, and promoting slow and consistent release of nutrients to the plants. Clearly, organic fertilizers are better, aren’t they?
Platelet-Rich Plasma is like organic fertilizers for our body.
Bonus: Strong Antimicrobial Properties
PRP’s healing function also has synergistic antimicrobial properties. A new study confirms that using Platelet-Rich Plasma in surgeries may have the potential to prevent infection and reduce the need for costly post-operative treatments. That’s a nice bonus for the organic fertilizer of our bodies. Perhaps there are more benefits to discover.
Conclusion
The scope of Platelet-Rich Plasma is growing as the scientific community continues to unearth its inherent properties. PRP is an unignorable and unavoidable component of healing.
- Published in Blog
7 PRP Treatments That Are Popular Right Now
TUESDAY, 10 APRIL 2018 / PUBLISHED IN BLOG
The time it takes to draw a patient’s blood, add a little citrate, and use a centrifugal machine with a PRP kit is only 15-20 minutes. This is the amount of time needed to create Platelet-Rich Plasma, or PRP. This can then be used for many purposes, including speeding up a patient’s recovery. PRP is by far the best healing agent that has growth factors and platelets to help with the healing process, which is also completely free and natural to obtain.
What are The Advantages Of Using PRP Correctly?
It is easy to create PRP simply by placing blood in a centrifuge, but it can have very few, if any, platelets and would otherwise be useless. However, with the right equipment, you can make PRP with up to 7x the amount of platelets. This can be amplified by using fat tissue and collagen fibers to create a PRP matrix.
7 Popular PRP Treatments
1. Facial Treatments
Many skin centers are thriving due to being one of the first to adopt PRP therapies. With the lack of side effects or downtime, it became incredibly popular. These treatments include wrinkle reduction, skin rejuvenation, dark circle and bag erasure, rosacea treatment, and even lip augmentation. One popular and generic treatment option includes combining PRP and a treatment known as microneedling. When this is applied, its effects are similar to Botox or facelifts, for far less cost and side effects.
2. Hair Loss
PRP growth factors can be beneficial when it comes to reversing non-genetic early-stage hair loss. Despite there being a huge market for this, almost no practitioners actually utilize it. Many clients have seen promise after hair thinning, and many have seen beard regrowth over time.
3. Arthritis and Cartilage
Arthritis treatments alone cost patients 6.4 billion dollars in 2013 for the US alone, with projections of up to 9 billion by the end of the decade. However, unlike other treatments, PRP is seen as the only treatment that can not just reduce symptoms but also regrow the cartilage. One of the most popular examples would be treatments for Temporomandibular Joint Osteoarthritis.
4. Anti-aging Properties
When it comes to the anti-aging market, there are endless treatments and procedures available. Yet, none of them even stand close to the effectiveness of PRP therapy. PRP combined with microneedling can be highly effective for stretch marks, acne scars, breast augmentation, and even skin conditions like Lichen Sclerosus.
5. Pain Relief and Musculoskeletal Healing
There are numerous treatments in this category, many of which are incredibly more effective than leading treatments. These include healing rotator cuffs, tennis elbow, Achilles tendonitis, patellar tendonitis, back pain, hip and pelvic problems, degenerative disc disease, golfer’s elbow, labral tear, bursitis, neck pain, avascular necrosis, and even pain related to nerve regeneration. Almost all of these treatments, unlike those in other categories on this list, also use ultrasound guidance when injecting the PRP directly into the affected tissue. This can allow patients to see fantastic results in as little as two weeks.
6. Fertility
Ovarian rejuvenation is where PRP is injected directly into a woman’s ovaries. This is meant to help reverse menopause and help lower fertility issues. This treatment can even be used for sexual regeneration. Although similar, this treatment is not the same as other treatments where PRP is injected into the vagina and is supposed to treat looseness, dryness, low sex drive, and incontinence.
7. COPD (Chronic Obstructive Pulmonary Disease)
Allergies, asthma, and COPD are among the growing list of conditions that PRP is being used to treat. For this to work, the PRP is mixed with a saline solution and then, using a nebulizer, inhaled, helping to regenerate lung tissue. Although it can take up to two months for patients to see the effects, many are seeing improvements. Almost 1 million people suffer from COPD a year, so anything that can help treat the condition is beneficial.
The Future of PRP
PRP has been trending rather well in recent years and seems to be here for the long term. Not only is it a fully natural remedy, but it is one that works better than most, if not all, traditional treatments. Many like it due to the fact that there are few side effects, it only takes a short amount of time, and there is no recovery period.
PRP has been adopted by thousands of clinics and practices throughout the US and the world. The demand for these treatments has been increasing almost faster than practices are choosing to provide them. Many patients are even willing to travel long distances just to receive these treatments.
So, are you providing PRP treatments yet?

- Published in Blog
How Foot and Ankle Surgeons Can Benefit From PRP
TUESDAY, 03 APRIL 2018 / PUBLISHED IN BLOG
Since it is a new science, many people are skeptical about Platelet-Rich Plasma, otherwise known as PRP. There are some studies out there that state that PRP works no better than a similarly administered placebo, but there are many other studies and doctors that claim that PRP works and works well. This also works well at a much lower cost and with fewer side effects than traditional medicine. One branch where the skepticism is loud and clear is podiatry, which deals with feet and ankles. Trying to combat this skepticism can help many surgeons to lower complication rates, improve patient satisfaction, and have better outcomes. For instance, here is a list of cases where PRP has been effective for the feet and ankles.
Plantar Fasciitis
PRP has become rather common as a treatment for Plantar Fasciitis, with many studies to prove the efficacy of this treatment. For instance, Dr. Daanial Kassicieh of Sarasota Neurology claims that PRP is one of the most effective treatments for this condition and that PRP can actually fully cure it. Many of his patients have avoided surgery just by utilizing PRP therapy. This is done with no downtime, no rehabilitation, and no side effects. This would explain why plantar fasciitis is the 5th most popular medical condition treated by PRP. This can be explained by the fact that over 3 million people are diagnosed with this condition and no other treatment really works for it besides, in fact, PRP.
Achilles Tendonitis
This is another condition that can be fairly hard to treat and gets worse over time unless healed. Many surgical approaches are often tricky and generally do not end up with good results. Because of this, the main treatment option is simply to give patients corticosteroids to reduce the pain, but really nothing else to treat the symptoms. However, there have been many studies done that have shown that PRP is a lot more effective, including those from the European Foot and Ankle Society. This means that PRP is a safer and more effective alternative than any other treatments available.
Diabetic Foot Ulcers
Diabetic foot ulcers can be troublesome, especially when they do not heal or heal properly. Over 2.5 million Americans with diabetes suffer from these ulcers. About 11% of these cases may need amputation of the affected limb. However, some studies have noted that just one injection of PRP and a topical solution bi-weekly started to heal the ulcers in just 8 weeks. Topical PRP has also been shown to work better than antiseptic creams as well.
Regenerating Bones
Bone regeneration is most commonly needed in the foot and ankle area. Although mechanical stabilization works best, the utilization of PRP has been surprising. PRP helps with healing bones and soft tissue at the damage site. According to a recent systematic review of 64 articles, the conclusion was to include more PRP therapy into the healing of foot and ankle bones. The science behind this is solid. For bone or tissue to form, three things are needed in the area:
- A scaffold for the growth to take place
- Biological stimulants to signal proteins
- Stem cells that provide bone-building potential
All three of these are crucial for bone formation. PRP can provide at least two of these, so there is no reason to ignore it when it comes to bone regeneration.
Ankle Sprains
This is an incredibly common condition and can be effectively treated by using PRP therapy. In one randomized controlled trial, researchers studied the effects of PRP injections on athletes with ankle sprains. This study showed that not only did PRP reduce the healing time by 20 days, but they also experienced much less pain. This can reduce the recovery period from 6 weeks to just about 2 or 3 weeks.
Immobilization is Vital
When it comes to foot and ankle-related injuries, one thing that really cannot be avoided is rest and rehabilitation. This is true regardless of whether PRP is administered. Because of this, many of the studies that show PRP to be ineffective often don’t use rest and rehabilitation, and that alone can be an issue. PRP is in no way a magic pill. All foot injuries need rest and rehabilitation in order to properly heal. With these two combined, it can drastically reduce healing times.
How Can Foot and Ankle Surgeons Benefit?
Using PRP in foot and ankle injuries is not going anywhere, so utilizing it would be the best way to go. Test it out with your patients, and try using platelet-rich plasma therapy instead of simply prescribing pills or doing costly surgeries. Your patients will thank you in the end.

- Published in Blog
Why Should you Include PRP In Your Medical Practice?
MONDAY, 26 MARCH 2018 / PUBLISHED IN BLOG
Platelet-Rich Plasma (PRP) has been a lifesaver for many medical practices, reigniting physicians’ passion for medicine. Not only is it 100% derived from the patient’s own body, but it is also natural and comes with minimal side effects. PRP can treat a wide range of medical conditions, often outperforming other treatment options.
The Simplicity of PRP
One of the most compelling reasons to include PRP in your practice is its simplicity. With an initial investment of about $1000, you can start offering PRP therapies. The equipment is relatively inexpensive and pays for itself quickly.
Long-Term Popularity
PRP is not a passing trend. It has been gaining popularity for years and shows no signs of slowing down. The market for PRP therapies is expected to reach nearly $500 million within the next decade, with an annual growth rate of 12.5% since 2015.
High Patient Satisfaction
Patient satisfaction is another significant advantage. In certain cases, satisfaction rates have been as high as 95%. Patients are often surprised by the efficacy of PRP, believing that their conditions could not be reversed or halted without side effects, downtime, and invasive surgeries.
Meeting the Growing Demand
Now is the time to start including PRP in your practice. The supply is low, but demand is booming. PRP therapies hold great promise, especially when combined with other treatments to increase efficacy. Since no standard has been established, you have the opportunity to set these standards yourself.
Be a Pioneer in PRP Therapy
It is vital that more doctors utilize PRP therapy to become pioneers in this field. PRP has the potential to revolutionize medicine, and missing out would not be a smart option.
Versatility Across Specialties
PRP can be utilized in almost every field and specialty, from sports medicine and pain management to skin rejuvenation, hair care, and even urology. Most physicians who use PRP treatments have also seen higher patient retention rates.
Conclusion: A Smart Addition to Your Practice
So, is there a legitimate reason not to add PRP to your practice? With its simplicity, high patient satisfaction, growing popularity, and versatility, PRP is a smart addition to any medical practice. Start offering PRP treatments and watch your practice thrive.

- Published in Blog
How To Choose A Platelet-Rich Plasma (PRP) Kit
MONDAY, 26 MARCH 2018 / PUBLISHED IN BLOG
Platelet-Rich Plasma (PRP) extraction methods have sparked debate due to varying reliability. Understanding how to select the best PRP kit can resolve these concerns and optimize treatment outcomes.
The Importance of Using a PRP Kit
Merely centrifuging blood in a test tube—often termed “bloody PRP”—is ineffective and may contain excessive red and white blood cells, potentially causing post-injection flare-ups. In contrast, PRP kits can concentrate platelets up to 5-7 times baseline levels, crucial for effective treatment.
Characteristics of a Good PRP Kit
Choosing the right PRP kit hinges on its ability to control platelet concentrations and eliminate unwanted cells, tailored to specific medical conditions.
Gel Separators
Kits with gel separators separate blood components via osmosis, retaining plasma and platelets while removing red and white blood cells. This method achieves modest platelet concentrations.
Buffy Coat
PRP kits that feature a buffy coat layer offer higher platelet concentrations (5-7 times baseline). The buffy coat, composed of platelets and white blood cells, is separated from red blood cells to minimize contamination.
Buffy Coat with Double Spin
Optimal for PRP quality, this kit further purifies the buffy coat by eliminating red blood cells through a second spin. This results in highly concentrated PRP with minimal red blood cell presence.
Biosafe Kit
Regarded as one of the best on the market, the Biosafe kit provides precise control over PRP production. It yields approximately 10cc of product, which can be double-spun for optimal platelet concentration. Users can customize the final product by choosing the inclusion or exclusion of red blood cells.
Understanding Leukocyte-Poor PRP
Leukocyte-poor PRP excludes white blood cells, which some believe may trigger inflammation and hinder growth factors. However, others argue that leukocytes are crucial for healing responses, promoting tissue regeneration and enhanced growth factor presence.
Choosing Filters for Leukocyte Reduction
To achieve leukocyte-poor PRP, practitioners can utilize Leukocyte Reduction (LR) filters like the CIF-LR filter, which efficiently separates white blood cells via electrostatic attraction. This ensures minimal clogging and filters out up to 99.99% of white blood cells.
Supporting Evidence for PRP
Despite skepticism, PRP’s efficacy is backed by extensive scientific research spanning decades and over 6000 studies. Patient willingness to pay out-of-pocket further underscores its perceived effectiveness, highlighting its growing popularity despite insurance coverage limitations.
Conclusion: Integrating PRP Into Practice
Choosing the right PRP kit is pivotal for optimizing treatment outcomes and patient satisfaction. With its proven benefits and increasing demand, integrating PRP into your medical practice offers a promising opportunity to enhance patient care and treatment efficacy.

- Published in Blog
Platelet-Rich Plasma (PRP) For Osteopathic Physicians
TUESDAY, 27 FEBRUARY 2018 / PUBLISHED IN BLOG
Although they can perform surgeries, osteopathic physicians try to avoid doing so whenever possible. Because of this, PRP seems to be an excellent fit for their practice. Since Osteopathy was built on the idea of self-healing, PRP seems to be a perfect fit.
The Current State of PRP Research
A while ago, PRP research was reviewed by The Journal Of The American Osteopathic Association, which concluded that more studies and evidence are needed to make a solid statement on its efficacy. Later, a case study was filed showcasing an 18-year-old high school football player who suffered from a sports injury. The case study showed that the muscle injury healed rapidly under PRP therapy. Although PRP is not yet universally acclaimed, it doesn’t mean Osteopathic Physicians can’t learn a lot or benefit from its use in their practice.
How Osteopathic Physicians Can Benefit From PRP
It’s Holistic
Osteopathic Physicians prefer to treat the patient rather than just treating a disease or its symptoms, making PRP a great fit. PRP works by using the body’s own resources and mechanics to help it heal itself over time. Instead of merely addressing symptoms like many conventional medicines do, it tackles the problem directly.
For example, there are cases where PRP therapy has taken the place of surgery and medication. Female patients have revived their sex drive after being treated for incontinence. While PRP therapy was initially pushed by allopathic doctors, it works wonders in Osteopathic medicine and can become a key treatment method for Osteopathic physicians.
Musculoskeletal Issues
In many practices, musculoskeletal pain is a common issue for Osteopathic Physicians. PRP is quickly becoming a primary treatment for these kinds of problems. For instance, many researchers believe PRP should be the main choice for patients suffering from knee meniscus issues.
In 2016, University of Missouri Doctor Patrick Smith published an FDA-sanctioned double-blind randomized placebo-controlled clinical trial on PRP. These trials are considered the gold standard in research. The study concluded that PRP provides safe and notable benefits for people suffering from knee osteoarthritis.
The Vast Potential of PRP
The third and most important reason why all physicians, including Osteopathic Physicians, should start using PRP therapy is its wide scope. Since PRP is simple and common, it’s safe to say that if PRP works on knee joints and tendons, it likely works on other tendons, joints, bones, and muscles. PRP will soon be a commonplace treatment for nearly all musculoskeletal diseases.
This means PRP has near limitless potential. This is especially important for Osteopathic Physicians because if a patient has a wrist problem, the main issue might appear further down the arm. Multiple PRP injections in various areas can not only heal the issue but also enhance other traditional methods used. This will help restore balance to the body and give full functionality back to the patient.
Success Stories and Expert Opinions
American Academy of Regenerative Medicine Doctor Peter Lewis has administered over 100,000 PRP injections to over 12,000 patients. He claims that more than 80% of his patients who have undergone PRP therapy have had fantastic results. Even patients who were candidates for surgery have benefited from PRP.
Are PRP Treatments FDA Approved?
As of this year, PRP treatments are not yet subject to FDA approval. This is because all treatments are performed on the same day as the extraction and use only materials already inside the patient’s body. Therefore, PRP therapy falls within the scope of the FDA Code of Federal Regulation title 21, part 1270, 1271.1, making it exempt from needing approval.

- Published in Blog
What is regenerative medicine?
TUESDAY, 30 JANUARY 2018 / PUBLISHED IN BLOG
Regenerative medicine is the exciting cutting-edge “medicine of the future” which holds the hope and promise of efficacy centered around the ability of human tissue to be repaired, replaced, and healed (regenerated) once human tissues and organs are damaged or diseased. Regenerative therapies aid and supplement the natural healing mechanisms of the body. These therapies often employ the activation of stem cells to stimulate the renewal of tissue damaged by injury, disease, or age. The rapid expansion of scientific knowledge offers great promise for continuing advances in this field of medicine, which holds vast potential to improve the quality of human life.
What are Stem Cells?
Stem cells are the basic building blocks of life. They are unspecialized cells that can produce more stem cells through mitosis or differentiate into specialized cells that carry out specific functions in the body. Stem cells are found throughout the body’s tissues, organs, and systems, although usually in small quantities in adults.
What are Hematopoietic Stem Cells?
Hematopoietic stem cells (HSCs) can give rise to all types of blood cells, including red blood cells, white blood cells, and platelets. They are particularly useful in the treatment of blood-related diseases and conditions.
What are Mesenchymal Stem Cells?
Mesenchymal Stem Cells (MSCs) are multipotent stromal cells that are non-blood-forming stem cells and can differentiate into a variety of cell types, including muscle, bone, cartilage, and fat cells.
When introduced into a patient’s body, MSCs can repair or replace damaged or degenerating tissue by communicating with the surrounding cells, causing a cellular cascade of healing (paracrine signaling).
The History and Potential of MSCs
Historically, the term MSC was coined in the late ’80s by the biomedical research authority, Dr. Arnold Caplan of Case Western Reserve. The acronym has recently been redefined by Caplan to “Medicinal Signaling Cell” since these cells secrete powerful bioactive molecules involved in cellular signaling and regeneration. Caplan now describes MSCs as a “multisite-regulatory dispensary” (Natural Drug Store).
The production of MSCs in the human body can be precipitated by bioactive placental tissues containing Growth Factors, Cytokines, and other powerful bioactive agents which trigger cell signaling.
The remarkable ability of MSCs makes them irreplaceable in medical treatments.
Accessible Sources of Stem Cells
Stem cells can be extracted from various parts of the body. They have been extracted from bone marrow and adipose tissue for a few decades. More recently, birth tissues from live births, including umbilical cord blood, cord tissue with Wharton’s Jelly, and amniotic membrane tissue, have been found to be a rich source of both HSCs and MSCs. These tissues precipitate target tissue production of MSCs through paracrine signaling. Growth Factors, Cytokines, Exosomes, and micro-RNA from birth tissues give rise to stem cells in this way. These cells, as well as MSCs contained in Wharton’s Jelly, tend to be more fit than adult stem cells.
Wharton’s Jelly
Wharton’s jelly is a gelatinous substance found in the umbilical cord, which is rich in stem cells. Studies have shown that mesenchymal stem cells (MSCs) have low immunogenicity. Human umbilical cord Wharton’s jelly provides a new source for MSCs that are highly proliferative and have multi-differentiation potential. Wharton’s Jelly Cells (WJCs) express MSC markers but low levels of human leukocyte antigen (HLA)-ABC and no HLA-DR. WJCs have low functional immunogenicity, and therefore recipient rejection has not been documented.
Advanced Regenerative Medicine
Advanced Regenerative Medicine involves the use of regenerative biomolecules, tissue engineering, and stem cells to treat diseased or injured tissues.

- Published in Blog
Photobiomodulation and why do we use a LED to irradiate PRP
Exploring the Power of Platelet-Rich Plasma (PRP) in Regenerative Medicine
WEDNESDAY, 14 MARCH 2018 / PUBLISHED IN BLOG
We have been in the regenerative medicine specialty for about 8 years. Like pretty much everyone, we started by using Platelet-Rich Plasma (PRP). We learned about it, were fascinated by it, and treated our patients with it. Patients loved it, and so did we.
The Versatility of PRP
PRP, if obtained and used correctly, is a very powerful tool to implement in any medical practice. It is especially useful for treating the elderly, osteoarthritis, wear and tear of tendons and ligaments, and loss of vitality. PRP is also frequently used in plastic and reconstructive surgery for wound care, scar improvement, and overall rejuvenation of the skin.
How Does PRP Work?
We are all familiar with platelets. They have significant power and influence over tissue regeneration. By concentrating them in a blood sample, we can obtain signaling proteins, cytokines, and growth factors. Adding white blood cells to the mix creates what is called L-PRP (leukocyte-rich PRP), making that “soup” even more potent.
Activating PRP for Maximum Benefits
To harness the power of these bioactive substances, we need to coax the cells into releasing them. Normally, platelets get activated by the addition of calcium or by contact with collagen. However, several studies have demonstrated the influence of low-intensity laser on the activity of some cells. This effect is called “Photobiomodulation.”
Understanding Photobiomodulation
Photobiomodulation is a form of light therapy that uses non-ionizing light sources, like LEDs or Helium-Neon lasers, to produce photochemical events at various biological scales. It has been demonstrated that this light interacts with the enzyme Cytochrome C oxidase, which is crucial in mitochondrial processes.
The Impact of Low-Level Laser Therapy
Several scientists studied this light and its effects on cellular cultures. They found that cells proliferate more when exposed to low-level laser and showed increased viability. We compared the levels of cytokines and growth factors in irradiated and non-irradiated samples. Sure enough, some growth factors even tripled in concentration after laser exposure. The famous Interleukin 10, an anti-inflammatory protein, doubled its levels, and endorphins were released in high levels.
Benefits of Photobiomodulation
The photobiomodulation process provides extraordinary benefits in pain management, inflammation reduction, immunomodulation, and promotion of wound healing and tissue regeneration. It plays a fundamental part in our protocols.
Conclusion
Isn’t it all amazing? The potential of PRP and photobiomodulation in regenerative medicine continues to astonish us. We will see you in the next blog. Keep your cells healthy!

- Published in Blog
IFATS Recommendations for FDA Regulation of Human Cells, Tissues, and Cellular and Tissue-Based Products
Introduction
The International Federation of Adipose Therapeutics and Sciences (IFATS) appreciates this opportunity to submit the following comments to supplement its earlier written comments and recent testimony at the September 12-13, 2016 Public Hearing on the 2014-2015 Draft HCT/P Guidances concerning: a) Minimal Manipulation; b) Same Surgical Procedure; c) Adipose Tissue; and d) Homologous Use.
IFATS Overview
International Federation of Adipose Therapeutics and Sciences (IFATS)
45 Lyme Road – Suite 304
Hanover, NH 03755 USA
Tel: 1-603-643-2325, Fax: 1-603-643-1444
Date: September 26, 2016
Addressed to:
Division of Dockets Management (HFA–305)
Food and Drug Administration
5630 Fishers Lane, Rm. 1061
Rockville, MD 20852
Re: FDA-2014-D-1856 – Comments to 2014-2015 Draft Guidance regarding:
- Docket FDA-2014-D-1584: “Same Surgical Procedure Exception under 21 CFR 1271.15(b): Questions and Answers Regarding the Scope of the Exception; Draft Guidance for Industry”
- Docket FDA-2014-D-1696: “Minimal Manipulation of Human Cells, Tissues, and Cellular and Tissue-Based Products; Draft Guidance for Industry and Food and Drug Administration Staff”
- Docket FDA-2014-D-1856: “Human Cells, Tissues, and Cellular and Tissue-Based Products from Adipose Tissue: Regulatory Considerations; Draft Guidance for Industry”
- Docket FDA-2015-D-3581: “Homologous Use of Human Cells, Tissues, and Cellular and Tissue-Based Products; Draft Guidance for Industry and FDA Staff”
Commitment to Advancing Adipose-Based Therapies
IFATS is committed to the responsible advancement of the science and translation of new adipose therapies, ensuring patient safety. Founded in 2003 by pioneering adipose stem cell biologists and clinician–scientists, IFATS aims to advance the science of adipose tissue biology and its clinical translation to therapeutic applications.
IFATS’s Global Influence and Expertise
Membership now spans 40 countries across North America, Europe, Africa, the Middle East, Asia, Australia, and Central and South America. It includes basic scientists, translational researchers, clinicians, and regulatory and biotech representatives. IFATS is aligned with prestigious journals, Stem Cells and Stem Cells Translational Medicine, and has contributed to defining adipose-derived cells in the publication Cytotherapy.
Review of FDA Draft Guidances
Drawing on this expertise, IFATS has reviewed the 4 draft guidances with great care. It respectfully requests the FDA to reconsider and modify the 4 draft HCT/P guidances as follows:
Recommendations
Recommendation #1: Cell-Based Risks
Interpret and evaluate an HCT/P’s homologous use and minimal manipulation based on its manufacturer’s intended use in the patient.
Recommendation #2: Provider-Based Risks
Reduce provider-created risks by targeting provider behavior.
Recommendation #3: Recognize Structural and Nonstructural Functions
Recognize that adipose HCT/Ps have both structural and nonstructural functions, and regulate based on its manufacturer’s intended use in the patient.
Recommendation #4: Revise Evaluation of Minimal Manipulation and Homologous Use
Revise the evaluation of minimal manipulation and homologous use as they pertain to particular applications of adipose tissue.
Conclusion
IFATS is committed to collaborating with the FDA to meet the challenges of regulating HCT/P therapies. We respectfully request a meeting with FDA representatives to discuss these issues and others related to the advancement and regulation of adipose-based therapies.
Respectfully submitted on behalf of IFATS,
Adam J. Katz, MD, FACS
Chair, IFATS Regulatory Affairs Committee & IFATS Co-Founder
University of Florida College of Medicine
Professor
Director of Plastic Surgery Research, Laboratory of BioInnovation and Translational Therapeutics
Division of Plastic Surgery, Department of Surgery
IFATS Board of Directors
- Bruce Bunnell, PhD – Tulane University / United States
- Louis Casteilla, PhD – University of Toulouse / France
- Sydney Coleman, MD – New York & Pittsburgh Universities / United States
- Julie Fradette, PhD – Lavalle University / Canada
- William Futrell, MD – Founders’ Board, University of Pittsburgh / United States
- Marco Helder, PhD – VU University Medical Center Amsterdam / The Netherlands
- Adam J. Katz, MD, FACS – Founders’ Board, University of Florida / United States
- Ramon Llull, MD, PhD – Founders’ Board, University of Barcelona / Spain
- Kacey Marra, PhD – University of Pittsburgh / United States
- Ricardo Rodriguez, MD – President (2016), Private Practice / Johns Hopkins / United States
- Peter Rubin, MD, FACS – Chair, Founders’ Board, Chairman of the Board, University of Pittsburgh / United States
- Stuart K. Williams, PhD – University of Louisville / United States
Members-at-Large
- Jeff Gimble, MD, PhD – Pennington Biomedical / United States
- Keith March, MD, PhD – Indiana University / United States
IFATS Recommendations for FDA Regulation of Human Cells, Tissues, and Cellular and Tissue-Based Products
Introduction
IFATS recognizes the FDA’s challenge in developing regulations that fulfill the agency’s dual and interrelated responsibilities of protecting patients while promoting innovation. Although these are complementary rather than competing objectives, they are often difficult to pursue simultaneously. The FDA’s 3-tiered, risk-based §§ 361 – 351 framework balances these concerns by making the degree of regulatory oversight proportionate to the degree of an HCT/P therapy’s risk.
Key Regulatory Concepts
The concepts of homologous use and minimal manipulation are key determinants of whether an HCT/P will be classified as a § 361 product (which does not need premarket approval) or a § 351 drug, device, and/or biological product (which requires formal premarket approval). The applicability of § 351’s “same surgical procedure” exception also turns on homologous use and minimal manipulation.
Challenges for Manufacturer-Clinicians
For most manufacturer-clinicians, § 351 categorization raises insurmountable obstacles due to the time and expense of obtaining premarket approval. In such cases, § 351 classification effectively prohibits access to safe and effective HCT/P therapies, even when those therapies involve a patient’s own cells and/or can deliver superior results with reduced risks. At the same time, § 351 oversight is essential for therapies that pose greater risks due to the HCT/P’s characteristics, mechanism(s) of action, and circumstances of use.
Addressing Provider Misconduct
A second type of risk involves rogue clinicians offering false promises in the form of unproven therapies performed with few safeguards and less training. Provider misconduct is not unique to HCT/P therapies; it pervades all areas of medical practice. Nevertheless, IFATS shares the FDA’s alarm over such practices in the context of HCT/Ps and is equally determined to curtail them. Effective regulation of HCT/P-related risks must recognize and respond to their multivariate causes. Put simply:
- Sections 351 and 361 appropriately attempt to regulate HCT/P therapies proportionate to the risks of unpredictable and/or unsafe cell behavior.
- However, the risks of untrained providers misusing HCT/P therapies are caused by providers misbehaving, not cells misbehaving.
Comprehensive Risk Management Strategy
Interpretive guidance that restricts the definition and application of HCT/P terminology can only go so far in restricting provider-based risks. Additionally, restrictive, inaccurate, or imprecise definitions and interpretations carry their own risks of restricting access to therapies and a patient’s right to evaluate risk through the process of informed consent. Therefore, IFATS recommends that the FDA adopt an overall two-part strategy that focuses on both categories of HCT/P risks: those relating to cell behavior and those that pertain to provider behavior.
Recommendations
Recommendation #1 – Cell-Based Risks
Interpret and evaluate an HCT/P’s homologous use and minimal manipulation based on its manufacturer’s intended use in the patient. Interpretive guidance should predicate each definition on the functions and/or characteristics of the specific composition (i.e., cell type(s) and/or matrix or other component(s)) that are involved in, and/or relevant to, the manufacturer-clinician’s intended use in the patient.
Recommendation #2 – Provider-Based Risks
To reduce provider-created risks, the FDA should target provider behavior by collaborating with IFATS and comparable organizations to draw on and supplement existing federal and state methods of certification, registration, and similar measures.
Detailed Explanation of Recommendations
Recommendation #1 – Cell-Based Risks
The four draft guidances on homologous use, minimal manipulation, same surgical procedure, and adipose tissue individually and collectively intend to “improve stakeholders’ understanding” of 21 CFR 1271 by clarifying the FDA’s interpretation of homologous use and minimal manipulation. As demonstrated by the initial round of public comments and the ensuing public hearing on September 12 and 13, 2016, the draft guidance documents have not clarified applicable regulations. They have instead compounded the difficulty of understanding and complying with them. The drafts’ introduction of new definitional inaccuracies has also amplified rather than reduced patient risk.
IFATS respectfully requests the agency to clarify the definitions and application of homologous use and minimal manipulation by interpreting each as referring to the characteristics of the specific cell type(s) and/or the matrix or other component(s) that are involved in, and/or relevant to, the manufacturer’s intended use in the patient.
Homologous Use Definition:
21 CFR 1271.3(c): Homologous use means the repair, reconstruction, replacement, or supplementation of a recipient’s cells or tissues with an HCT/P that performs the same basic function or functions in the recipient as in the donor.
Recommended Guidance:
As used in this section, “performs the same basic function or functions in the recipient as in the donor” shall be interpreted as referring to one or more of the functions of the specific composition of the therapeutic/product, reflecting the specific cell type(s) and/or the specific matrix or other component(s) in the donor tissue that are involved in, and/or relevant to, the manufacturer’s intended use in the patient.
Minimal Manipulation Definition:
21 CFR 1271.3(f) Minimal manipulation means:
- For structural tissue, processing that does not alter the original relevant characteristics of the tissue relating to the tissue’s utility for reconstruction, repair, or replacement;
- For cells or nonstructural tissues, processing that does not alter the relevant biological characteristics of cells.
Recommended Guidance:
As used in this section, “relevant” characteristics shall be interpreted to mean the characteristics of the specific cell type(s) and/or the specific matrix or other component(s) in the donor tissue that are involved in, and/or relevant to, the manufacturer’s intended use in the patient.
Rationale:
Incorporating and relying on the manufacturer’s intended use harmonizes the interpretation and definition of homologous use and minimal manipulation with statutory directives to predicate the regulation of drugs, devices, and biologics on the manufacturer’s intended use. Defining relevant characteristics in terms of “the characteristics of specific cell type(s) and/or the matrix or other component(s) in the donor tissue that are involved in, and/or relevant to the manufacturer’s intended use in the patient” promotes patient safety by insisting on a reasonable and scientifically supportable rationale for using an HCT/P for a particular mechanism of action. This clarification balances the FDA’s dual responsibilities of protecting patients from undue safety risks while promoting the ongoing availability and continued development of HCT/P therapies.
Example of Non-Homologous Use:
Decellularized adipose matrix used to accomplish the manufacturer’s intended use of a particular metabolic or systemic effect in the patient (e.g., reducing insulin levels in a diabetic patient) is non-homologous because decellularized matrix is not relevant to metabolic or systemic activity.
Conclusion
Adopting this two-part strategy can control risk more comprehensively—and therefore more effectively—in furtherance of the FDA’s dual and interrelated obligations of protecting patients and promoting the availability of HCT/P therapies.
Introduction to FDA Regulations and IFATS Recognition
IFATS acknowledges the FDA’s dual role in patient protection and innovation promotion within the HCT/P sector. Balancing these objectives is crucial yet challenging.
Understanding the FDA’s Risk-Based Framework
The FDA’s § 361 – § 351 framework categorizes HCT/P therapies based on risk levels, influenced by concepts like homologous use and minimal manipulation.
Impact of Regulatory Classification on Access to HCT/P Therapies
Homologous use and minimal manipulation determine whether an HCT/P falls under § 361 (no premarket approval needed) or § 351 (requires premarket approval), affecting accessibility and innovation.
Provider Misconduct Risks in HCT/P Therapies
Rogue clinicians offering unproven therapies pose significant risks. Addressing provider behavior is essential for patient safety and regulatory efficacy.
IFATS Recommendations for Risk Mitigation
Recommendation #1 – Cell-Based Risks: Interpreting Homologous Use and Minimal Manipulation
IFATS proposes clarifying homologous use and minimal manipulation definitions based on manufacturer-intended use, enhancing regulatory clarity and patient safety.
Recommendation #2 – Provider-Based Risks: Targeting Provider Behavior
Collaboration with IFATS and other bodies to enhance certification and monitoring mechanisms can mitigate risks associated with provider misconduct effectively.
Recommendation #3 – Regulatory Scope for Adipose HCT/Ps
Expanding the definition of adipose tissue to include both structural and nonstructural functions aligns with biological accuracy and regulatory intent.
Conclusion: Enhancing Patient Safety and Access to HCT/P Therapies
IFATS urges the FDA to adopt a comprehensive strategy that addresses both cell-based and provider-based risks to uphold patient safety and foster innovation in HCT/P therapies.
Regulating an HCT/P’s Risks Based on Manufacturer’s Intended Use
Regulating the risks of Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/Ps) is crucially tied to their intended use and mechanisms of action in patients. This ensures effective regulatory oversight and evaluation.
Regulatory Framework: §§ 351-361
The regulatory oversight of HCT/Ps under §§ 351-361 hinges on assessing the product’s risk level. Central to this determination are the criteria of homologous use and minimal manipulation.
Homologous Use Defined (21 CFR 1271.3(c))
Homologous use is defined as the repair, reconstruction, replacement, or supplementation of a recipient’s cells or tissues with an HCT/P that performs the same basic function as in the donor.
Minimal Manipulation Criteria (21 CFR 1271.3(f))
Minimal manipulation of structural tissue involves processing that preserves the tissue’s original characteristics essential for its utility in repair, reconstruction, or replacement. For nonstructural tissues, it preserves relevant biological characteristics.
Impact on Adipose Tissue
The classification of adipose tissue as exclusively structural neglects its nonstructural functions, limiting evaluation under § 361 criteria and obstructing risk assessment.
Same Surgical Procedure Exception
The § 351 “same surgical procedure” exception applies only to HCT/Ps meeting homologous use and minimal manipulation criteria, impacting nonstructural adipose applications.
Recommendation #4: Revising Evaluation Criteria
IFATS urges the FDA to reconsider specific adipose tissue applications concerning homologous use and minimal manipulation criteria.
Example A: Decellularizing Adipose Tissue
Decellularization of adipose tissue for structural use should be recognized as minimal manipulation under §§ 351 and 361 guidelines.
Example B: Structural Use of Fat in Breast Surgery
Applying adipose tissue for breast augmentation should be considered homologous use due to its structural function in restoring form and shape.
Example C: Stromal Vascular Fraction (SVF) for Nonstructural Use
SVF extraction from adipose tissue retains nonstructural components crucial for nonstructural applications, meeting minimal manipulation and homologous use criteria.
Conclusion and Call to Action
IFATS requests the FDA to amend draft guidance on HCT/Ps to align with scientific understanding and clinical practices of adipose tissue applications.
References
- Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: A joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy. 2013;15:641-648
- Diaz-Flores L, Gutierrez R, Madrid JF, Varela H, Valladares F, Acosta E, Martin-Vasallo P, Diaz-Flores L, Pericytes. Morphofunction, interactions and pathology in a quiescent and activated mesenchymal cell niche. Histol Histopathol. 2009;24:909-969
- Gimble The function of adipocytes in the bone marrow stroma. The New Biologist. 1990;2:304-312
- Cawthorn WP, Scheller EL, Learman BS, Parlee SD, Simon BR, Mori H, Ning X, Bree AJ, Schell B, Broome Bone marrow adipose tissue is an endocrine organ that contributes to increased circulating adiponectin during caloric restriction. Cell metabolism. 2014;20:368-375
- Meunier P, Aaron J, Edouard C, VlGNON Osteoporosis and the replacement of cell populations of the marrow by adipose tissue: A quantitative study of 84 iliac bone biopsies. Clinical orthopaedics and related research. 1971;80:147-154
- N. Über die wiederanheilung vollstädig vom körper getrennter, die ganze fettschicht en- thaltender hautstucke. Zbl f Chir 1893;30:16-17
- Hollander E, Joseph Cosmetic surgery. Handbuch der Kosmetik. Leipzig, Germany: Veriag von Velt. 1912;688
- Miller Cannula implants and review of implantation technics in esthetic surgery: In two parts. Oak Press; 1926.
- Gimble JM Fat circadian biology. Journal of applied physiology. 2009;107:1629-1637
- Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R, Richards GJ, Campfield LA, Clark FT, Deeds Identification and expression cloning of a leptin receptor, ob-r. Cell. 1995;83:1263-1271
- Salgado AJ, Gimble Secretome of mesenchymal stem/stromal cells in regenerative medicine.
Biochimie. 2013;95:2195
- Salgado AJ, Reis RL, Sousa N, Gimble Adipose tissue derived stem cells secretome: Soluble factors and their roles in regenerative medicine. Curr Stem Cell Res Ther. 2009
- Khan M, Joseph Adipose tissue and adipokines: The association with and application of adipokines in obesity. Scientifica. 2014;2014
- Vicennati V, Garelli S, Rinaldi E, Di Dalmazi G, Pagotto U, Pasquali Cross-talk between
adipose tissue and the hpa axis in obesity and overt hypercortisolemic states. Hormone molecular biology and clinical investigation. 2014;17:63-77
- Kargi AY, Iacobellis Adipose tissue and adrenal glands: Novel pathophysiological mechanisms and clinical applications. International journal of endocrinology. 2014;2014
- Maïmoun L, Georgopoulos NA, Sultan Endocrine disorders in adolescent and young female athletes: Impact on growth, menstrual cycles, and bone mass acquisition. The Journal of Clinical Endocrinology
& Metabolism. 2014;99:4037-4050
- McIntosh K, Zvonic S, Garrett S, Mitchell JB, Floyd ZE, Hammill L, Kloster A, Di Halvorsen Y, Ting JP,
Storms RW. The immunogenicity of human adipose‐derived cells: Temporal changes in vitro. Stem cells. 2006;24:1246-1253
- McIntosh KR, Frazier T, Rowan BG, Gimble Evolution and future prospects of adipose- derived immunomodulatory cell therapeutics. Expert review of clinical immunology. 2013;9:175-184
- McIntosh KR, Lopez MJ, Borneman JN, Spencer ND, Anderson PA, Gimble Immunogenicity of allogeneic adipose-derived stem cells in a rat spinal fusion model. Tissue Engineering Part A. 2009;15:2677-2686
- Mitchell JB, McIntosh K, Zvonic S, Garrett S, Floyd ZE, Kloster A, Di Halvorsen Y, Storms RW, Goh B, Kilroy G. Immunophenotype of human adipose‐derived cells: Temporal changes in stromal‐associated and stem cell–associated markers. Stem cells. 2006;24:376-385
- Gimble JM, Dorheim MA, Cheng Q, Medina K, Wang CS, Jones R, Koren E, Pietrangeli C, Kincade Adipogenesis in a murine bone marrow stromal cell line capable of supporting b lineage lymphocyte growth and proliferation: Biochemical and molecular characterization. European journal of immunology. 1990;20:379-387
- Frazier TP, McLachlan JB, Gimble JM, Tucker HA, Rowan Human adipose-derived stromal/stem cells induce functional cd4+ cd25+ foxp3+ cd127− regulatory t cells under low oxygen culture conditions. Stem cells and development. 2014;23:968-977
- Frazier TP, Gimble JM, Kheterpal I, Rowan Impact of low oxygen on the secretome of human adipose- derived stromal/stem cell primary cultures. Biochimie. 2013;95:2286-2296
- Miranville A, Heeschen C, Sengenes C, Curat C, Busse R, Bouloumie Improvement of postnatal neovascularization by human adipose tissue-derived stem cells. Circulation. 2004;110:349-355
- Rehman J, Traktuev D, Li J, Merfeld-Clauss S, Temm-Grove CJ, Bovenkerk JE, Pell CL, Johnstone BH, Considine RV, March Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004;109:1292-1298
- Planat-Benard V, Silvestre J-S, Cousin B, André M, Nibbelink M, Tamarat R, Clergue M, Manneville C, Saillan-Barreau C, Duriez Plasticity of human adipose lineage cells toward endothelial cells physiological and therapeutic perspectives. Circulation. 2004;109:656-663
- Kilroy GE, Foster SJ, Wu X, Ruiz J, Sherwood S, Heifetz A, Ludlow JW, Stricker DM, Potiny S, Green P, Halvorsen YD, Cheatham B, Storms RW, Gimble Cytokine profile of human adipose-derived stem cells: Expression of angiogenic, hematopoietic, and pro- inflammatory factors. J Cell Physiol. 2007;212:702-709
- Ribeiro CA, Fraga JS, Grãos M, Neves NM, Reis RL, Gimble JM, Sousa N, Salgado The secretome of stem cells isolated from the adipose tissue and wharton jelly acts differently on central nervous system derived cell populations. Stem Cell Res Ther. 2012;3:18
- Silva NA, Gimble JM, Sousa N, Reis RL, Salgado Combining adult stem cells and olfactory ensheathing cells: The secretome effect. Stem cells and development. 2013;22:1232-1240
- Cho YJ, Song HS, Bhang S, Lee S, Kang BG, Lee JC, An J, Cha CI, Nam DH, Kim. Therapeutic effects of human adipose stem cell‐conditioned medium on stroke. Journal of neuroscience research. 2012;90:1794-1802
- Egashira Y, Sugitani S, Suzuki Y, Mishiro K, Tsuruma K, Shimazawa M, Yoshimura S, Iwama T, Hara The conditioned medium of murine and human adipose-derived stem cells exerts neuroprotective effects against experimental stroke model. Brain research. 2012;1461:87-95
- Wei X, Du Z, Zhao L, Feng D, Wei G, He Y, Tan J, Lee WH, Hampel H, Dodel Ifats collection:The conditioned media of adipose stromal cells protect against hypoxia‐ischemia‐induced brain damage in neonatal rats. Stem Cells. 2009;27:478-488
- Wei X, Zhao L, Zhong J, Gu H, Feng D, Johnstone B, March K, Farlow M, Du Adipose stromal cells-secreted neuroprotective media against neuronal apoptosis. Neuroscience letters. 2009;462:76-79
- Zhao L, Wei X, Ma Z, Feng D, Tu P, Johnstone B, March K, Du Adipose stromal cells- conditional medium protected glutamate-induced cgns neuronal death by bdnf. Neuroscience letters. 2009;452:238-240
- Cousin B, André M, Arnaud E, Pénicaud L, Casteilla Reconstitution of lethally irradiated mice by cells isolated from adipose tissue. Biochemical and biophysical research communications. 2003;301:1016-1022
- Han J, Koh YJ, Moon HR, Ryoo HG, Cho CH, Kim I, Koh Adipose tissue is an extramedullary reservoir for functional hematopoietic stem and progenitor cells. Blood.2009
- Harms M, Seale Brown and beige fat: Development, function and therapeutic potential. Nature medicine. 2013;19:1252-1263
- Rahman S, Lu Y, Czernik PJ, Rosen CJ, Enerback S, Lecka-Czernik Inducible brown adipose tissue, or beige fat, is anabolic for the skeleton. Endocrinology. 2013;154:2687-2701
- Wu J, Cohen P, Spiegelman Adaptive thermogenesis in adipocytes: Is beige the new brown? Genes & development. 2013;27:234-250
- Krings A, Rahman S, Huang S, Lu Y, Czernik P, Lecka-Czernik Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone. 2012;50:546-552
- van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JM, Kemerink GJ, Bouvy ND, Schrauwen P, Teule Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009;360:1500-1508
- Peirce V, Carobbio S, Vidal-Puig The different shades of fat. Nature. 2014;510:76-83
- Enerbäck S, Gimble Lipoprotein lipase gene expression: Physiological regulators at the transcriptional and post-transcriptional level. Biochimica et Biophysica Acta (BBA)- Lipids and Lipid Metabolism. 1993;1169:107-125
- Rudolph MC, Neville MC, Anderson Lipid synthesis in lactation: Diet and the fatty acid switch. Journal of mammary gland biology and neoplasia. 2007;12:269-281
- Gimble JM, Katz AJ, Bunnell Adipose-derived stem cells for regenerative medicine. Circ Res. 2007;100:1249-1260
- Bellows CF, Zhang Y, Chen J, Frazier ML, Kolonin Circulation of progenitor cells in obese and lean colorectal cancer patients. Cancer Epidemiology Biomarkers & Prevention. 2011;20:2461- 2468
- Bellows CF, Zhang Y, Simmons PJ, Khalsa AS, Kolonin Influence of bmi on level of circulating progenitor cells. Obesity. 2011;19:1722-1726
- Krijnen PA NB, Meinster E, Vo K, Musters RJ, Kamp O, Niessen HW,, Juffermans LJ. Acute myocardial infarction does not affect functional characteristics of adipose derived stem cells in rats, but reduces the number of stem cells in adipose tissue. IFATS Annual Meeting. 2014:100
- Traktuev DO, Merfeld-Clauss S, Li J, Kolonin M, Arap W, Pasqualini R, Johnstone BH,March KL. A population of multipotent cd34-positive adipose stromal cells share pericyte and mesenchymal surface markers, reside in a periendothelial location, and stabilize endothelial networks. Circulation research. 2008;102:77-85
- Traktuev DO, Prater DN, Merfeld-Clauss S, Sanjeevaiah AR, Saadatzadeh MR, Murphy M, Johnstone BH, Ingram DA, March Robust functional vascular network formation in vivo by cooperation of adipose progenitor and endothelial cells. Circulation research. 2009;104:1410-1420
- Merfeld-Clauss S, Gollahalli N, March KL, Traktuev Adipose tissue progenitor cells directly interact with endothelial cells to induce vascular network formation. Tissue Engineering Part A. 2010;16:2953-2966
- Merfeld-Clauss S, Lupov IP, Lu H, Feng D, Compton-Craig P, March KL, Traktuev. Adipose stromal cells differentiate along a smooth muscle lineage pathway upon endothelial cell contact via induction of activin a. Circulation research. 2014;115:800-809
- Crisan M, Yap S, Casteilla L, Chen C-W, Corselli M, Park TS, Andriolo G, Sun B, Zheng B, Zhang A perivascular origin for mesenchymal stem cells in multiple human organs. Cell stem cell. 2008;3:301-313
- Ter Horst E, Naaijkens B, Krijnen P, Van Der Laan A, Piek J, Niessen Induction of a monocyte/macrophage phenotype switch by mesenchymal stem cells might contribute to improved infarct healing postacute myocardial infarction. Minerva cardioangiologica. 2013;61:617-625
- Guisantes E, Fontdevila J, Rodríguez Autologous fat grafting for correction of unaesthetic scars. Annals of plastic surgery. 2012;69:550-554
- Klinger M, Caviggioli F, Klinger FM, Giannasi S, Bandi V, Banzatti B, Forcellini D, Maione L, Catania B, Vinci Autologous fat graft in scar treatment. Journal of Craniofacial Surgery. 2013;24:1610-1615
- Klinger M, Marazzi M, Vigo D, Torre Fat injection for cases of severe burn outcomes: A new perspective of scar remodeling and reduction. Aesthetic plastic surgery. 2008;32:465-469
- Khouri RK, Smit JM, Cardoso E, Pallua N, Lantieri L, Mathijssen IM, Khouri Jr RK, Rigotti Percutaneous aponeurotomy and lipofilling: A regenerative alternative to flap reconstruction? Plastic and reconstructive surgery. 2013;132:1280-1290
- Balkin DM, Samra S, Steinbacher Immediate fat grafting in primary cleft lip repair. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2014;67:1644-1650
- Rigotti G, Marchi A, Galie M, Baroni G, Benati D, Krampera M, Pasini A, Sbarbati. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: A healing process mediated by adipose-derived adult stem cells. Plastic and reconstructive surgery. 2007;119:1409-1422
- Villani F, Caviggioli F, Klinger F, Klinger Rehabilitation of irradiated head and neck tissues by autologous fat transplantation. Plastic and reconstructive surgery. 2009;124:2190-2191
- Chang CC, Thanik VD, Lerman OZ, Saadeh PB, Warren SM, Coleman SR, Hazen Treatment of radiation skin damage with coleman fat grafting. STEM CELLS. 2007;25:3280-3281
- Sultan SM, Stern CS, Allen Jr RJ, Thanik VD, Chang CC, Nguyen PD, Canizares O, Szpalski C, Saadeh PB, Warren Human fat grafting alleviates radiation skin damage in a murine model. Plastic and reconstructive surgery. 2011;128:363-372
- Loder S, Peterson JR, Agarwal S, Eboda O, Brownley C, DeLaRosa S, Ranganathan K, Cederna P, Wang SC, Levi Wound healing after thermal injury is improved by fat and adipose-derived stem cell isografts. Journal of Burn Care & Research. 2015;36:70-76
- Sultan SM, Barr JS, Butala P, Davidson EH, Weinstein AL, Knobel D, Saadeh PB, Warren SM, Coleman SR, Hazen Fat grafting accelerates revascularisation and decreases fibrosis following thermal injury. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2012;65:219-227
- Cuomo R, Zerini I, Botteri G, Barberi L, Nisi G, D’ANIELLO Postsurgical pain related to breast implant: Reduction with lipofilling procedure. In Vivo. 2014;28:993-996
- Maione L, Vinci V, Caviggioli F, Klinger F, Banzatti B, Catania B, Lisa A, Klinger Autologous fat graft in postmastectomy pain syndrome following breast conservative surgery and radiotherapy. Aesthetic plastic surgery. 2014;38:528-532
- Caviggioli F, Maione L, Forcellini D, Klinger F, Klinger Autologous fat graft in postmastectomy pain syndrome. Plastic and reconstructive surgery. 2011;128:349-352
- Caviggioli F, Vinci V, Codolini Autologous fat grafting: An innovative solution for the treatment of post-mastectomy pain syndrome. Breast Cancer. 2013;20:281-282
- Salgarello M, Visconti The role of sacrolumbar fat grafting in the treatment of spinal fusion instrumentation-related chronic low back pain: A preliminary report. Spine. 2014;39:E360-E362
- Faroni A, Terenghi G, Reid Adipose-derived stem cells and nerve regeneration: Promises and pitfalls. Int Rev Neurobiol. 2013;108:121-136
- Vaienti L, Gazzola R, Villani F, Parodi Perineural fat grafting in the treatment of painful neuromas. Techniques in hand & upper extremity surgery. 2012;16:52-55
- Marangi GF, Pallara T, Cagli B, Schena E, Giurazza F, Faiella E, Zobel BB, Persichetti Treatment of early-stage pressure ulcers by using autologous adipose tissue grafts. Plastic Surgery International. 2014;2014
- Lolli P, Malleo G, Rigotti Treatment of chronic anal fissures and associated stenosis by autologous adipose tissue transplant: A pilot study. Diseases of the Colon & Rectum. 2010;53:460-466
- Cantarella G, Baracca G, Forti S, Gaffuri M, Mazzola Outcomes of structural fat grafting for paralytic and non-paralytic dysphonia. Acta Otorhinolaryngologica Italica. 2011;31:154
- DeFatta RA, DeFatta RJ, Sataloff Laryngeal lipotransfer: Review of a 14-year experience. Journal of Voice. 2013;27:512-515
- Sataloff Autologous fat implantation for vocal fold scar. Current opinion in otolaryngology & head and neck surgery. 2010;18:503-506
- Cantarella G, Mazzola RF, Mantovani M, Baracca G, Pignataro Treatment of velopharyngeal insufficiency by pharyngeal and velar fat injections. Otolaryngology– Head and Neck Surgery. 2011;145:401-403
- Papa N, Luca G, Sambataro D, Zaccara E, Maglione W, Gabrielli A, Fraticelli P, Moroncini G, Beretta L, Santaniello A. Regional implantation of autologous adipose tissue-derived cells induces a prompt healing of long-lasting indolent digital ulcers in patients with systemic sclerosis. Cell transplantation. 2014
- Hovius SE, Kan HJ, Smit X, Selles RW, Cardoso E, Khouri Extensive percutaneous aponeurotomy and lipografting: A new treatment for dupuytren disease. Plastic and reconstructive surgery. 2011;128:221-228
- Verhoekx JS, Mudera V, Walbeehm ET, Hovius Adipose-derived stem cells inhibit the contractile myofibroblast in dupuytren’s disease. Plastic and reconstructive surgery. 2013;132:1139-1148
- Bank J, Fuller SM, Henry GI, Zachary Fat grafting to the hand in patients with raynaud phenomenon: A novel therapeutic modality. Plastic and reconstructive surgery. 2014;133:1109-1118
- Damgaard OE, Siemssen Lipografted tenolysis. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2010;63:e637-e638
- Colonna M, Scarcella M, d’Alcontres F, Delia G, Lupo Should fat graft be recommended in tendon scar treatment? Considerations on three cases (two feet and a severe burned hand). European review for medical and pharmacological sciences. 2014;18:753-759
- Merikanto JE, Alhopuro S, Ritsilä Free fat transplant prevents osseous reunion of skull defects: A new approach in the treatment of craniosynostosis. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 1987;21:183-188
- Mojallal A, Lequeux C, Shipkov C, Breton P, Foyatier J-L, Braye F, Damour Improvement of skin quality after fat grafting: Clinical observation and an animal study. Plastic and reconstructive surgery. 2009;124:765-774
- Lockwood Superficial fascial system (sfs) of the trunk and extremities: A new concept. Plastic and reconstructive surgery. 1991;87:1009-1018
- Song AY, Askari M, Azemi E, Alber S, Hurwitz DJ, Marra KG, Shestak KC, Debski R, Rubin Biomechanical properties of the superficial fascial system. Aesthetic Surgery Journal. 2006;26:395-403
- Flynn The use of decellularized adipose tissue to provide an inductive microenvironment for the adipogenic differentiation of human adipose-derived stem cells. Biomaterials. 2010;31:4715-4724
- Brown BN, Freund JM, Han L, Rubin JP, Reing JE, Jeffries EM, Wolf MT, Tottey S, Barnes CA, Ratner Comparison of three methods for the derivation of a biologic scaffold composed of adipose tissue extracellular matrix. Tissue Engineering Part C: Methods. 2011;17:411-421
- Wu I, Nahas Z, Kimmerling KA, Rosson GD, Elisseeff An injectable adipose matrix for soft tissue reconstruction. Plastic and reconstructive surgery. 2012;129:1247
- Omidi E, Fuetterer L, Mousavi SR, Armstrong RC, Flynn LE, Samani Characterization and assessment of hyperelastic and elastic properties of decellularized human adipose tissues. Journal of biomechanics. 2014;47:3657-3663
- Wang L, Johnson JA, Zhang Q, Beahm Combining decellularized human adipose tissue extracellular matrix and adipose-derived stem cells for adipose tissue engineering. Acta biomaterialia. 2013;9:8921-8931
- Healy C, Allen Sr The evolution of perforator flap breast reconstruction: Twenty years after the first diep flap. Journal of reconstructive microsurgery. 2014;30:121-125
- LoTempio MM, Allen Breast reconstruction with sgap and igap flaps. Plastic and reconstructive surgery. 2010;126:393-401
- Erić M, Mihić N, Krivokuća Breast reconstruction following mastectomy; patient’s satisfaction. Acta Chir Belg. 2009;109:159-166
- Diaz-Flores L, Gutierrez R, Lizartza K, et Behavior of In Situ Human Native Adipose Tissue CD34+ Stromal/Progenitor Cells During Different Stages of Repair. Tissue-Resident CD34+ Stromal Cells as a Source of Myofibroblasts. Anatomical record. 2014.
- Gil-Ortega M, Garidou L, Barreau C, et Native adipose stromal cells egress from adipose tissue in vivo: evidence during lymph node activation. Stem cells. 2013;31(7):1309-20.

- Published in Blog
Purest Liver-like Cells to Date Generated from Induced Pluripotent Stem Cells (iPSCs)
SATURDAY, 01 OCTOBER 2016 / PUBLISHED IN BLOG
Researchers from the Medical University of South Carolina (MUSC) and the University of Pennsylvania have discovered a new methodology for purifying liver cells generated from induced pluripotent stem cells (iPSCs) that could facilitate progress toward an important clinical goal: treating patients with disease-causing liver mutations by transplanting unmutated liver cells derived from their own stem cells.
Background on Liver Cell Generation from iPSCs
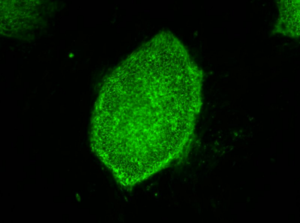
Credit: Image courtesy of Stephen A. Duncan, Ph.D., at the Medical University of South Carolina
Previous attempts to generate liver-like cells from stem cells have yielded heterogeneous cell populations with little similarity to diseased livers in patients.
The Role of the Next Generation Genetic Association Studies Program
The National Heart, Lung, and Blood Institute (NHLBI)’s Next Generation Genetic Association Studies Program (Next Gen) was created to bank stem cell lines sourced from patients in genome-wide association studies (GWAS). The goal of the Next Gen Lipid Conditions sub-section, a collaborative effort between Stephen A. Duncan, Ph.D., chair of regenerative medicine at MUSC, and Daniel J. Rader, M.D., and Edward E. Morrisey, Ph.D., both at the University of Pennsylvania, is to help determine the genetic sources of heart, lung, or blood conditions that also include the liver.
Genome-Wide Association Studies (GWAS)
GWAS studies map the genomes in hundreds of people to look for genetic mutation patterns that differ from the genomes of healthy individuals. As GWAS studies map more genomes, they become more likely to find the correct genetic mutations that cause a disease. Once a panel of suspected mutations is built, stem cells from these individuals can be manipulated in culture dishes to differentiate into any of the body’s cells. The cells can be screened to learn more about the mutations and to test panels of drugs that might ultimately help treat patients harboring a disease.
Challenges in Cell Manipulation Process
Problems arise during the cell manipulation process. For example, iPSCs persistently refuse to mature uniformly into liver-like cells when fed growth factors. Traditionally, antibodies have been used to recognize features of maturity on the surfaces of cells and purify cells that are similar, an approach that has been crucial to stem cell research. But available antibodies that recognize mature liver cells are scanty and tend to recognize many different kinds of cells. The many types of cells in mixed populations have diverse characteristics that can obscure underlying disease-causing genetic variations, which tend to be subtle.
Introduction of Chemo Proteomic Cell Surface Capture (CSC) Technology
Instead of relying on antibodies, Duncan and his team embraced a new technology called chemo proteomic cell surface capture (CSC) technology. CSC technology allowed the researchers to map the most highly produced proteins on the surface of liver cells during the final stages of differentiation of stem cells into liver cells. The most abundant protein was targeted with an antibody labeled with a fluorescent marker and used to sort the mature liver cells from the rest.
Successful Generation of Pure Liver-like Cells
The procedure was highly successful: The team had a population of highly pure, homogeneous, and mature liver-like cells. Labeled cells had far more similar traits of mature hepatocytes than unlabeled cells. Pluripotent stem cells that had not differentiated were excluded from the group of labeled cells.
“That’s important,” says Duncan. “If you’re wanting to transplant cells into somebody that has liver disease, you really don’t want to be transplanting pluripotent cells because pluripotent cells form tumors called teratocarcinomas.”
Future Implications
Duncan cautioned that transplantation of iPSC-derived liver cells is not yet ready for translation to the clinic, but the technology for sorting homogeneous liver cells can be used now to successfully and accurately model and study disease in the cell culture dish.
“We think that the ability to generate pure populations will get rid of the variability, and therefore really help us combine with GWAS studies to identify allelic variations that are causative of a disease, at least in the liver,” he says.
Contributions to the Study
Researchers at the University of Minnesota (Minneapolis) and the Medical College of Wisconsin (Milwaukee) contributed to the study, published August 25, in Stem Cell Reports.

- Published in Blog












