Natural Killer (NK) cells are essential components of the innate immune system, emerging as key players in immune surveillance, antiviral defense, tissue modulation, and advanced therapeutic applications. In regenerative medicine, their role transcends cytotoxicity, offering promising therapeutic potential for inflammatory, oncologic, autoimmune, and degenerative conditions. This article provides a detailed overview of NK cell ontogeny, activation mechanisms, functional regulation, clinical strategies, and translational challenges associated with their use in advanced cellular immunotherapy.
1. Introduction and Ontogeny
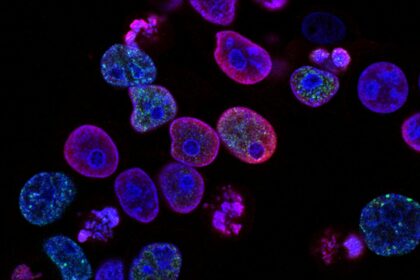
NK cells are large granular lymphocytes derived from CD34+ hematopoietic progenitors in the bone marrow. They are classified within the innate immune system due to their ability to recognize infected or malignant cells without prior antigen sensitization.
Differentiation and Subtypes
Two main NK subpopulations exist in peripheral blood:
- CD56^bright CD16⁻ NK cells: ~10% of circulating NKs. Potent cytokine producers (IFN-γ, TNF-α) with immunomodulatory functions.
- CD56^dim CD16⁺ NK cells: ~90% of circulating NKs. Highly cytotoxic via perforin- and granzyme-mediated apoptosis.
NK cells develop mainly in the bone marrow but also in secondary lymphoid organs (fetal liver, lymph nodes, tonsils, uterus). Their differentiation is driven by key cytokines such as IL-15, IL-2, IL-21, and the transcription factor Eomes.
2. Activation, Inhibition, and Cytotoxic Mechanisms
NK cell function is tightly regulated by a balance between activating and inhibitory receptors:
Inhibitory Receptors
- KIRs (Killer Immunoglobulin-like Receptors): recognize HLA-C and HLA-B.
- NKG2A/CD94: binds HLA-E.
- These receptors prevent NK cell activation against healthy, MHC-I expressing cells.
Activating Receptors
- NKG2D: detects stress ligands (e.g., MIC-A/B, ULBPs) on transformed or infected cells.
- Natural Cytotoxicity Receptors (NCRs): NKp30, NKp44, NKp46.
- CD16 (FcγRIII): mediates Antibody-Dependent Cellular Cytotoxicity (ADCC), essential for synergy with monoclonal antibody therapies.
Effector Mechanisms
- Direct cytotoxicity: release of perforins and granzymes inducing apoptosis.
- ADCC: lysis of antibody-coated target cells.
- Cytokine production: IFN-γ, TNF-α, GM-CSF to enhance innate and adaptive responses.
3. Clinical Applications in Oncologic Immunotherapy
3.1 Autologous vs Allogeneic NK Cells
- Autologous NK cells: isolated, expanded, and reinfused into the same patient. Safe but may be suppressed by the patient’s tumor microenvironment.
Allogeneic NK cells (haploidentical or off-the-shelf): bypass self-tolerance mechanisms, enhancing cytotoxicity in a controlled manner. More effective in eliminating tumor cells lacking self-MHC expression.
3.2 CAR-NK Cells
Chimeric Antigen Receptor (CAR)-NK cells combine NK cell innate properties with antigen-specific targeting:
- Lower risk of cytokine release syndrome (CRS) than CAR-T.
- Minimal risk of graft-versus-host disease (GvHD).
- Universal application via NK-92 cell lines or umbilical cord blood.
Early-phase trials have shown over 70% response rates in hematological malignancies and some solid tumors, with favorable safety profiles.
4. Role in Regenerative Medicine and Immune Modulation
4.1 Control of Inflammatory Microenvironments
NK cells modulate sterile or pathological inflammation by interacting with macrophages (M1/M2), dendritic cells, and regulatory T cells, promoting:
- Resolution of chronic inflammation.
- Tissue regeneration via immune modulation.
- A conducive environment for stem cells and tissue engineering therapies.
4.2 Anti-Aging Applications
Restoring NK cell function in aging individuals or using young donor NKs may:
- Enhance immune surveillance.
- Promote clearance of senescent cells (senolytic effect).
- Improve tissue repair in liver, muscle, skin, and vasculature.
4.3 Combination with Other Cell Therapies
Co-culturing or co-infusing NK cells with MSCs, MUSE cells, or exosomes can:
- Reduce tumorigenic risks in iPSC-based therapies.
- Protect allogeneic grafts via immune buffering.
- Accelerate neovascularization and neurorepair.
5. GMP Production, Expansion, and Clinical Validation
Sources and Expansion Methods
- Peripheral blood: requires leukapheresis and IL-2/IL-15-driven expansion.
- Umbilical cord blood: source of naïve, immunologically “clean” NK cells.
- NK-92 cell line: immortalized, modifiable, and suitable for large-scale therapy.
GMP Processing
- Magnetic isolation (CD56+/CD3-), expansion, activation.
- Cryopreservation, lot tracking, quality documentation.
- Rigorous testing for endotoxins, sterility, viability (>85%), and function.
Quality Control and Potency Assays
- In vitro cytotoxicity assays: against K562, Jurkat, or Daudi cells.
- Phenotyping: CD16, NKG2D, CD69, NKp46, perforin, granzyme B via flow cytometry.
- Secretome analysis: cytokine profiling (IFN-γ, TNF-α).
6. Challenges and Future Perspectives
| Challenge | Ongoing Strategies |
| Short in vivo persistence | IL-15 superagonists, nanoparticle delivery, CAR |
| Tumor immunosuppression | TGF-β blockade, PD-1/PD-L1 inhibition |
| Industrial scalability | Bioreactors, NK-92 lines, off-the-shelf models |
| Personalized application | KIR/HLA genotyping for tailored therapies |
Natural Killer cells represent a paradigm shift in modern immunotherapy. Their innate cytotoxicity, immune modulatory capabilities, and favorable safety profile make them ideal candidates for advanced clinical applications, especially in oncology, regenerative medicine, and aging-related conditions.
ISSCA supports ongoing clinical research, medical training, and translational implementation of NK cell-based therapies as part of a comprehensive approach to next-generation regenerative medicine.




