To improve the on-page SEO for the article on James P. Allison and his work in immunotherapy, here are suggested H2 headings and optimizations:
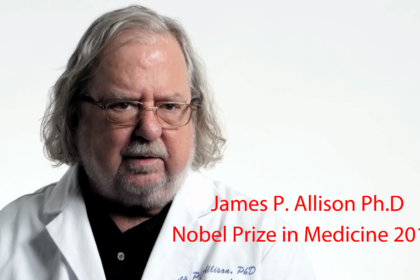
Introduction to James P. Allison, PhD
James P. Allison, Chair of the Department of Immunology and Director of the Immunotherapy Platform at MD Anderson Cancer Center, has dedicated his career to revolutionizing cancer treatment.
Early Influences and Motivations
Losing his mother to lymphoma and two uncles to melanoma and lung cancer deeply influenced Allison’s decision to pursue cancer research.
Focus on T Cells and Immunotherapy
Allison’s interest in T cells, pivotal warriors of the immune system, sparked during his undergraduate studies at the University of Texas at Austin.
Development of Checkpoint Blockade Antibodies
Allison’s breakthrough involved preventing immune “brakes” from engaging, allowing T cells to continue attacking and eliminating tumors.
Impact of Ipilimumab (Yervoy) on Melanoma Treatment
Ipilimumab, developed by Allison’s team, significantly extended survival rates for patients with metastatic melanoma.
Advancements in PD-1 Blockade Therapy
Further developments in PD-1 blockade therapies have expanded treatment options for various cancers including head and neck, lung, kidney, and bladder cancers.
Future Directions in Immunotherapy Research
Allison’s lab continues to explore combinations of checkpoint blockades to optimize treatment responses across different cancer types.
Integration of Immunotherapy with Traditional Treatments
While not replacing traditional therapies, Allison believes immunotherapy will become integral to comprehensive cancer treatment strategies.
Conclusion: The Future of Immunotherapy
James P. Allison’s contributions have transformed cancer care, offering hope for longer and improved quality of life for cancer patients worldwide.
Share Your Insights
What are your thoughts on the impact of immunotherapy in cancer treatment? Share your experiences and opinions.
Final Thoughts
Understanding the pioneering work of James P. Allison sheds light on the transformative potential of immunotherapy in oncology.
These headings help organize the content for better SEO and readability, highlighting key aspects of James P. Allison’s career and his contributions to cancer research and immunotherapy.




